What are Leaky Guts Symptoms in How to Fix It ?
Welcome, Wellness Warriors, to another in-depth exploration into the intricate world of our bodies. Today, we tackle a topic that has garnered significant attention in recent years within the wellness community: Leaky Gut Syndrome.
While not yet a recognized medical diagnosis in all mainstream circles, the concept of increased intestinal permeability – often referred to as “leaky gut” – is a well-researched phenomenon with profound implications for our overall health. In this comprehensive guide, we will dissect what leaky gut syndrome is, its potential links to various health conditions, and most importantly, the actionable steps you can take to foster gut healing and restore your digestive vitality.
What Exactly is Leaky Gut Syndrome? The Science Behind Intestinal Permeability
To understand leaky gut, we must first appreciate the remarkable architecture of our digestive system, particularly the gastrointestinal tract. Imagine your gut as a highly selective gatekeeper. Its primary role is to allow essential nutrients to pass from our food into our bloodstream while simultaneously preventing harmful substances, toxins, and undigested food particles from entering our circulation. This selective barrier is formed by the intestinal lining, a single layer of specialized cells called epithelial cells.
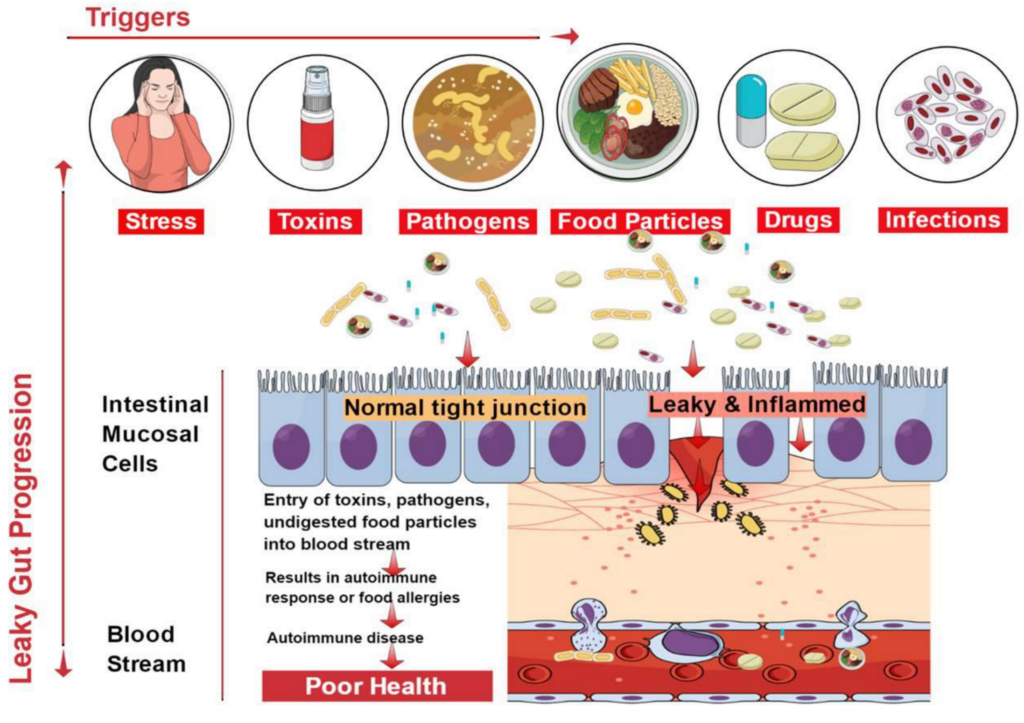
These epithelial cells are held together by structures known as tight junctions. Think of these as microscopic seals that regulate what passes through the intestinal walls. In a healthy individual, these tight junctions are, well, tight, ensuring a robust gut barrier function. However, in individuals with leaky gut syndrome, these tight junctions become compromised, allowing the intestinal lining to become more permeable. This increased gut permeability means that the gate is no longer as selective, permitting various undesirable elements to “leak” into the bloodstream.
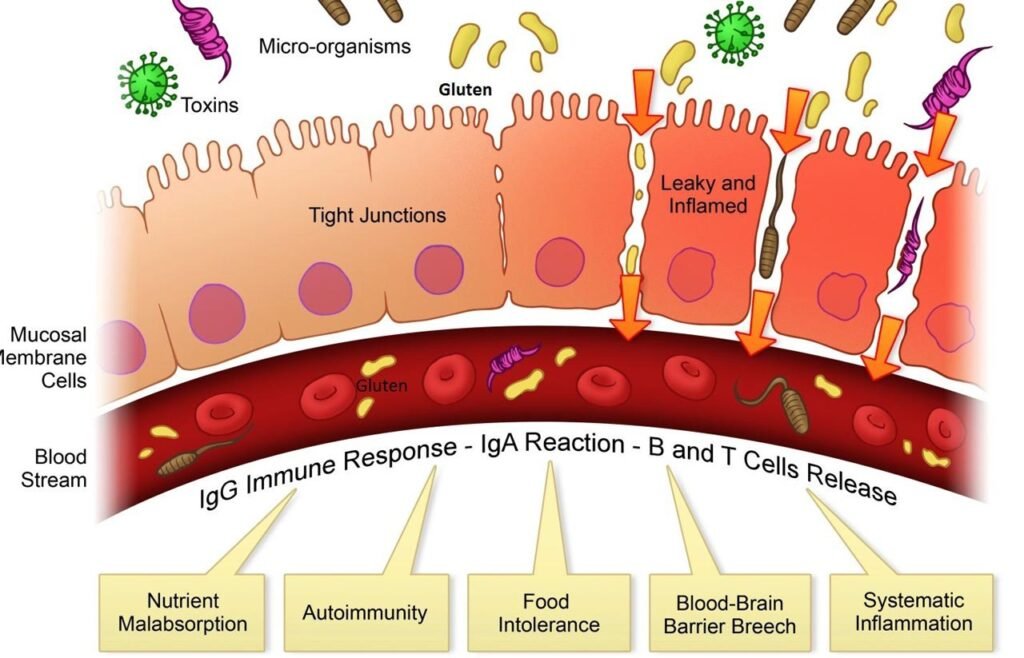
When these unwanted substances, such as toxins, bacteria (bad bacteria), and incompletely digested food components, enter the bloodstream, our immune system perceives them as foreign invaders. This triggers an immune response, leading to widespread chronic inflammation throughout the body. Over time, this persistent low-grade inflammation can contribute to a cascade of health conditions.
While the medical community may still debate its status as a standalone disease, the scientific evidence supporting the concept of increased intestinal permeability is robust. Clinical studies have explored its role in a multitude of conditions, moving it beyond a mere wellness buzzword to a subject of serious scientific inquiry.
The Ripple Effect: Health Conditions Linked to Leaky Guts
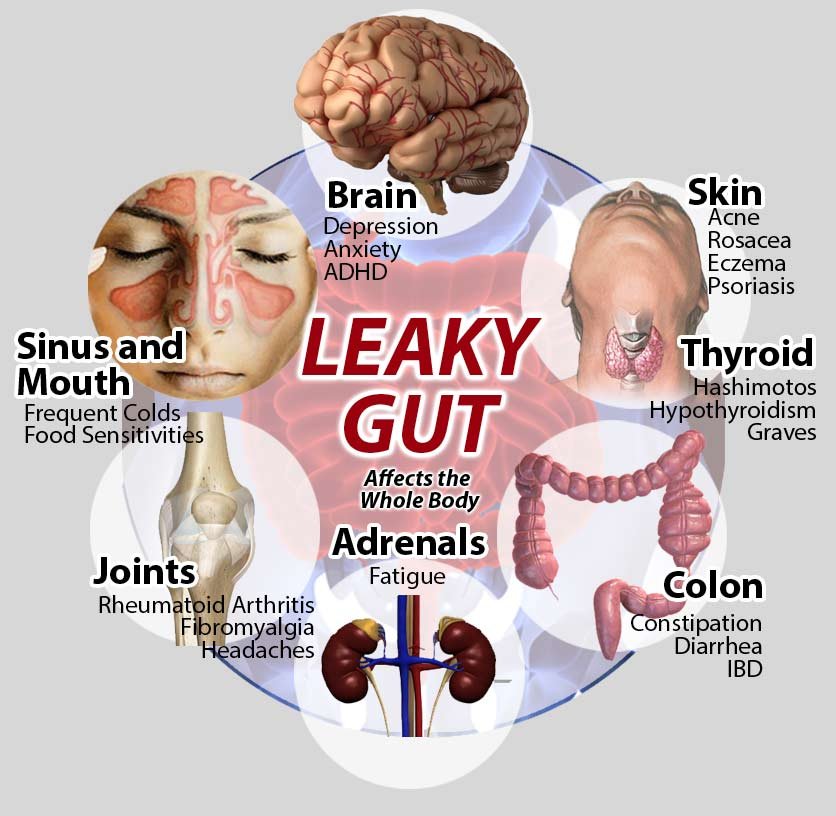
The chronic inflammation initiated by a compromised gut lining can manifest in a surprising array of symptoms and medical conditions far beyond mere digestive issues. While research is ongoing to fully elucidate the cause-and-effect relationships, many functional medicine practitioners and a growing number of traditional healthcare providersrecognize the significant role of gut permeability in several chronic ailments.
Here are some of the key health conditions that have been linked to increased intestinal permeability:
- Autoimmune Diseases: Perhaps one of the most compelling connections is with autoimmune diseases. When the immune system is constantly activated by substances leaking from the gut, it can, in some susceptible individuals, begin to mistakenly attack the body’s own tissues. Conditions like celiac disease (a severe form of gluten sensitivity), rheumatoid arthritis, Type 1 diabetes, and even some thyroid conditions are being actively investigated for their ties to increased gut permeability. While celiac disease directly damages the lining of the small intestine, research suggests that even non-celiac gluten sensitivity might contribute to leaky gut in some individuals.
- Inflammatory Bowel Disease (IBD): Both Crohn’s disease and ulcerative colitis, the two main forms of inflammatory bowel disease, are characterized by chronic inflammation of the digestive tract. While not the sole cause, increased intestinal permeability is frequently observed in individuals with IBD and is considered a significant contributing factor to the ongoing inflammatory processes and digestive symptoms such as abdominal pain.
- Irritable Bowel Syndrome (IBS): Often mistaken for IBD, irritable bowel syndrome is a functional gastrointestinal disorder characterized by a range of digestive problems including abdominal pain, bloating, constipation, and diarrhea. While the exact mechanisms are complex, research suggests that alterations in gut permeability and the gut microbiome may play a role in the symptoms experienced by many with IBS.
- Food Sensitivities and Food Allergies: A permeable gut wall can allow larger undigested food particles to enter the bloodstream, leading to an exaggerated immune response to certain foods. This can manifest as food sensitivities (which are delayed, less severe reactions) or, in some cases, exacerbate existing food allergies. Common culprits often include dairy products and gluten.
- Systemic Symptoms: Beyond the gut, leaky gut syndrome can contribute to a variety of systemic symptoms that often baffle traditional diagnoses. These can include:
- Chronic fatigue syndrome: The constant immune activation and inflammation can drain energy levels.
- Joint pain: Systemic inflammation can affect joints, leading to discomfort similar to that seen in autoimmune conditions like rheumatoid arthritis.
- Skin issues: Conditions like eczema and psoriasis have been linked to gut health.
- Brain fog and mood disturbances: The gut-brain axis is a complex system, and an unhealthy gut can impact neurotransmitter production and brain function.
It’s crucial to understand that leaky gut is often an underlying cause or an underlying condition that contributes to the development or severity of these issues rather than being the sole disease itself. Therefore, addressing gut permeabilitycan be a vital component of a holistic treatment plan.
READ MORE: What to Eat for Your Gut Health? [ Gut-healing Guide ]
What Causes the Gut to “Leak”? Understanding the Risk Factors

Several factors can contribute to the breakdown of the intestinal barrier function and lead to increased gut permeability. These risk factors often interact, creating a perfect storm for the development of leaky gut syndrome:
- Poor Diet: The standard Western diet, high in processed foods, refined sugars, unhealthy fats, and low in dietary fiber, is a major culprit. These foods can promote the growth of bad bacteria in the gut microbiome, leading to an imbalance known as dysbiosis, and directly damage the intestinal lining.
- Chronic Stress: We often underestimate the power of the mind-gut connection. Chronic stress has a profound impact on the digestive system, altering gut flora composition and increasing gut permeability. The constant release of stress hormones can directly compromise the tight junctions.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics, and corticosteroids can all disrupt the gut microbiome and damage the intestinal lining with prolonged use.
- Toxins: Exposure to environmental toxins, pesticides, and certain chemicals can also contribute to gut damage.
- Infections: Bacterial, viral, or parasitic infections in the gut can directly harm the gut lining. Small intestinal bacterial overgrowth (SIBO), where an excessive amount of bacteria colonizes the small intestine, is a common contributing factor to leaky gut.
- Nutrient Deficiencies: Deficiencies in certain essential nutrients like Vitamin D, zinc, and Vitamin A can impair the integrity of the intestinal lining and the function of the immune system.
- Alcohol Consumption: Excessive alcohol intake can directly irritate and damage the gut lining.
The Good News: How to Fix Leaky Gut Syndrome
The good news is that while the concept of leaky gut can seem daunting, the intestinal lining has an incredible capacity for regeneration and gut healing. By addressing the underlying cause of increased gut permeability and implementing targeted strategies, many individuals experience significant improvements in their digestive health and overall well-being. There’s no single “fastest way” or “best way” to fix it, as it requires a multi-faceted approach.
Here’s a comprehensive treatment plan focusing on diet, lifestyle, and targeted supplementation:
1. Dietary Changes: The Foundation of Gut Healing

Transforming your dietary choices is the single most powerful step you can take. The goal is to remove foods that irritate the gut and introduce foods that nourish and repair the intestinal lining.
- Eliminate Inflammatory Foods: This is often the first and most crucial step. Temporarily remove common culprits that can contribute to inflammation and gut permeability. These include:
- Gluten: Found in wheat, barley, and rye. Even if you don’t have celiac disease, many people experience non-celiac gluten sensitivity that can irritate the gut.
- Dairy products: Lactose and casein can be problematic for many.
- Refined sugars: Feed bad bacteria and promote inflammation.
- Processed foods: Often contain artificial ingredients, unhealthy fats, and lack beneficial nutrients.
- Unhealthy fats: Trans fats and excessive omega-6 fatty acids (found in many vegetable oils) can promote inflammation.
- Alcohol: Irritates the gut lining.
- Embrace Gut-Friendly Foods: Focus on a nutrient-dense, whole-foods diet that supports gut healing.
- Bone broth: Rich in collagen, gelatin, and amino acids like glutamine, which are crucial for repairing the gut wall and reducing inflammation. It’s often considered one of the pillars of a gut healing diet.
- Fermented foods: Sauerkraut, kimchi, kefir, and kombucha are excellent sources of beneficial bacteria that help rebalance the gut microbiome.
- High-fiber foods: Plenty of fruits, vegetables, and whole grains (if tolerated) provide dietary fiber that acts as prebiotics, feeding your beneficial bacteria.
- Healthy fats: Incorporate sources of omega-3 fatty acids like wild-caught salmon, chia seeds, flaxseeds, and avocados. These have anti-inflammatory properties.
- Lean proteins: Organic, grass-fed meats, poultry, and fish provide essential amino acids for tissue repair.
- Plenty of water: Hydration is crucial for all bodily functions, including digestion.
- Consider a Specific Diet: For some, a more structured approach like the Autoimmune Protocol (AIP) diet or a low-FODMAP diet might be beneficial, especially if symptoms are severe or there’s an existing underlying condition like SIBO. However, it’s essential to work with a healthcare provider or a registered dietitian when implementing such restrictive diets to ensure adequate nutrient intake.
2. Lifestyle Modifications: Beyond the Plate
Diet is paramount, but lifestyle factors play a vital role in gut healing.
- Manage Stress Levels: As mentioned, chronic stress is a significant contributor to leaky gut. Incorporate stress-reducing practices into your daily routine:
- Mindfulness and meditation
- Yoga or tai chi
- Spending time in nature
- Adequate sleep (7-9 hours per night)
- Deep breathing exercises
- Prioritize Sleep: Lack of sleep can disrupt the gut microbiome and increase inflammation. Aim for consistent, quality sleep.
- Regular Exercise: Moderate exercise can improve gut motility and reduce inflammation. However, avoid overtraining, which can increase stress levels.
3. Targeted Supplementation: Strategic Support

While a nutrient-dense diet is the cornerstone, certain supplements can provide strategic support for gut healing. Always consult with a healthcare provider or a functional medicine practitioner before starting any new supplement regimen.
- Probiotic Supplement: A high-quality probiotic supplement can help restore a healthy balance of gut flora by introducing beneficial bacteria. Look for multi-strain probiotics with a high CFU count.
- Digestive Enzymes: For those with impaired nutrient absorption or digestive problems, digestive enzymes taken with meals can help break down food more efficiently, reducing the burden on the gut and potentially lessening the amount of undigested food particles that can contribute to leakage.
- L-Glutamine: An amino acid that is a primary fuel source for intestinal cells and plays a crucial role in maintaining the integrity of the intestinal lining.
- Zinc: Essential for maintaining the integrity of tight junctions.
- Vitamin D: Plays a vital role in immune function and gut barrier integrity.
- Omega-3 Fatty Acids: Supplementing with fish oil can provide concentrated anti-inflammatory benefits.
- Collagen/Gelatin: Can support the repair of the gut lining.
- Slippery Elm and Marshmallow Root: These herbs have soothing properties that can help calm irritated intestinal walls.
Diagnosis and the Road Ahead: Working with a Healthcare Provider

While there isn’t one single blood test universally recognized for definitively diagnosing leaky gut, some tests can provide clues about intestinal permeability and related issues. These might include:
- Lactulose/Mannitol Test: This test measures how well two non-metabolized sugars are absorbed. Increased absorption of larger sugar molecules suggests increased gut permeability.
- Zonulin Levels: Zonulin is a protein that regulates tight junctions. Elevated levels can indicate increased intestinal permeability. However, its clinical utility as a standalone diagnostic marker is still under investigation.
- Comprehensive Stool Analysis: This can provide insights into the balance of your gut microbiome, presence of pathogens, and markers of inflammation.
- Food Sensitivity Testing: While controversial as a definitive diagnostic tool for allergies, these tests can sometimes highlight immune reactions to specific foods that may be contributing to leaky gut symptoms.
It’s important to reiterate that “leaky gut syndrome” is not yet a universally recognized medical diagnosis in mainstream medicine, and some medical community members remain skeptical. However, the underlying concept of increased intestinal permeability is backed by scientific evidence and numerous human studies and clinical trials.
The key is to work with a healthcare provider who understands the concept of gut permeability and its impact on overall health. Many integrative and functional medicine practitioners specialize in this area and can help you develop a personalized treatment plan based on your unique symptoms, medical history, and, if appropriate, specific test results. For example, the Cleveland Clinic acknowledges the concept of intestinal permeability and its implications, often discussing it within the context of related digestive problems.
Conclusion: Empowering Your Gut for Lifelong Wellness

Leaky Gut Syndrome, or increased intestinal permeability, is more than just a fleeting wellness trend; it’s a fundamental aspect of digestive health with far-reaching implications for our entire body. By understanding the intricate workings of our gut lining and the factors that can compromise its integrity, we empower ourselves to take proactive steps towards vibrant health.
The journey to gut healing requires commitment, patience, and often dietary changes, but the potential rewards – from improved digestion and increased energy levels to reduced inflammation and a bolstered immune system – are immeasurable. Remember, your gut is your second brain, a complex ecosystem that plays a vital role in every aspect of your well-being. By nurturing your gut health, you’re not just fixing a symptom; you’re building a foundation for lifelong wellness.
Stay informed, stay empowered, and keep fighting for your health, Wellness Warriors!